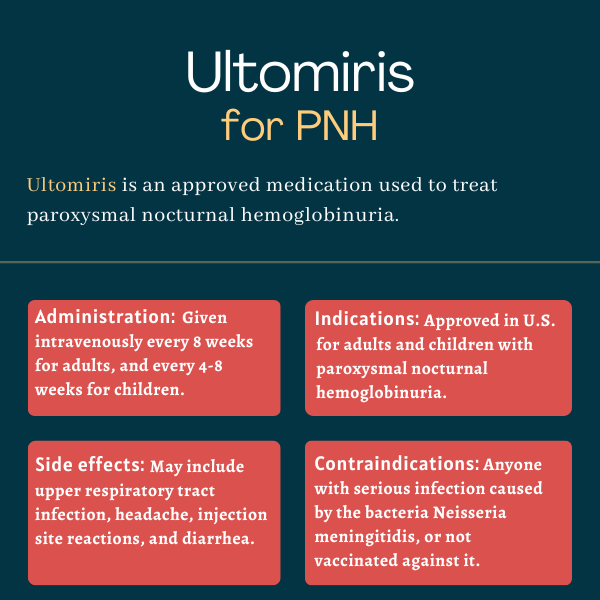
Ultomiris (ravulizumab) for paroxysmal nocturnal hemoglobinuria
What is Ultomiris for PNH?
Ultomiris (ravulizumab-cwvz) is a complement inhibitor that’s approved for the treatment of adults and children with paroxysmal nocturnal hemoglobinuria (PNH). It’s given by an into-the-vein (intravenous) infusion or an under-the-skin (subcutaneous) injection.
The therapy was originally developed by Alexion Pharmaceuticals, which was acquired by AstraZeneca in 2021.
Ultomiris also is approved for the treatment of adults and children with atypical hemolytic uremic syndrome, and as a therapy for adults with generalized myasthenia gravis.
Therapy Snapshot
| Brand Name: | Ultomiris |
| Chemical Name: | ravulizumab-cwvz |
| Usage: | treatment of paroxysmal nocturnal hemoglobinuria |
| Administration: | into-the-vein (intravenous) infusion and under-the-skin (subcutaneous) injection |
How does Ultomiris work?
PNH is a rare disorder characterized by the premature death of red blood cells, a process known as hemolysis. Most cases of PNH result from mutations in the PIGA gene in hematopoietic stem cells, which are stem cells that give rise to all blood cells in the body.
The PIGA gene provides instructions for making the phosphatidylinositol glycan class A (PIG-A) protein, which is involved in the formation of a molecule that’s known as a GPI anchor — fully, a glycophosphatidylinositol (GPI) anchor. As its name suggests, this molecule works as an anchor, attaching many different proteins to the surface of cells. These proteins, called GPI-anchored proteins, play several important roles.
Mutations in PIGA lead to the complete or partial loss of two GPI-anchored proteins, CD55 and CD59. These proteins are key inhibitors of the complement cascade, a part of the immune system. Deficiencies of CD55 and CD59 cause the complement system to attack and destroy red blood cells.
One of the steps in complement activation is the cleavage or splitting of a protein called C5 into two subunits, C5a and C5b. Ultomiris is designed to bind to complement protein C5 and prevent its cleavage, thereby reducing complement-mediated hemolysis in people with PNH. By doing so, it can help control disease symptoms.
Ultomiris’ mechanism of action is similar to that of Soliris (eculizumab), another approved PNH therapy also developed by Alexion. However, according to the company, Ultomiris is designed to last longer in the body, allowing for less frequent dosing. With maintenance infusions given once every two months, patients may require 6-7 Ultomiris infusions per year — 20 fewer infusions compared with Soliris.
Who with PNH can take Ultomiris?
Ultomiris was approved by the U.S. Food and Drug Administration in 2018 for the treatment of adults with PNH. That approval was extended to children, ages 1 month and older, in 2021.
In the European Union, the therapy was first approved to treat adults with PNH in 2019. This approval also was expanded to children, based on their weight, and adolescents in 2021. To be prescribed Ultomiris, young children must weigh 10 kg (22 pounds) or more.
In the U.S., Ultomiris is only available through a restricted access program under a Risk Evaluation and Mitigation Strategy (REMS) due to the risk of serious meningococcal infections associated with the treatment. The access program is called Ultomiris REMS. Patients must be carefully monitored for signs of meningococcal infections, as these can become rapidly life-threatening or fatal if not detected and treated early.
Who should not take Ultomiris?
Ultomiris should not be taken by people who:
- have a serious infection caused by Neisseria meningitidis, the bacteria that causes a serious illness called meningococcal disease
- are not vaccinated against Neisseria meningitidis, unless the risk of delaying treatment with Ultomiris is greater than the risk of a meningococcal infection.
How is Ultomiris administered in PNH?
Ultomiris is given by an intravenous or into-the-vein infusion, or via a subcutaneous or under-the-skin injection. Subcutaneous administration is approved for maintenance dosing in adult patients only.
Intravenous administration
Patients are given an initial infusion, called a loading dose, followed by maintenance doses for as long as treatment lasts. A supplemental dose is required if patients are undergoing plasma exchange therapy or receiving intravenous immunoglobulin (IVIg), as these procedures have been shown to lower Ultomiris levels in the blood.
The first maintenance dose is given two weeks after the loading dose. In the case of those switching from subcutaneous to intravenous Ultomiris, the first into-the-vein maintenance dose should be given one week after the last under-the-skin maintenance dose.
Subsequent maintenance doses are given every eight weeks (two months) for adults, and every four or eight weeks (one or two months) for children, depending on body weight.
When administered intravenously, Ultomiris dosing varies according to body weight:
- For PNH patients weighing 5 to less than 10 kg (11 to less than 22 pounds), the loading dose is 600 mg and maintenance doses are 300 mg, given every four weeks.
- For those weighing 10 to less than 20 kg (22 to less than 44 pounds), both the loading dose and maintenance doses are 600 mg, with maintenance doses being given every four weeks.
- For patients weighing 20 to less than 30 kg (44 to less than 66 pounds), the loading dose is 900 mg and maintenance doses are 2,100 mg, given every eight weeks.
- For those weighing 30 to less than 40 kg (66 to less than 88 pounds), the loading dose is 1,200 mg and maintenance doses are 2,700 mg, given every eight weeks.
- For patients weighing 40 to less than 60 kg (88 to less than 132 pounds), the loading dose is 2,400 mg and maintenance doses are 3,000 mg, given every eight weeks.
- For those weighing 60 to less than 100 kg (132 to less than 220 pounds), the loading dose is 2,700 mg and maintenance doses are 3,300 mg, given every eight weeks.
- For those weighing 100 kg (220 pounds) or more, the loading dose is 3,000 mg and maintenance doses are 3,600 mg, given every eight weeks.
Subcutaneous administration
For subcutaneous injection, the treatment is available in a single-dose prefilled cartridge containing a translucent, clear to yellowish color solution of 245 mg/3.5 mL (70 mg/mL). It is meant to be used only with a supplied single-use on-body injector.
The recommended subcutaneous maintenance dose is 490 mg once weekly in adults weighing 40 kg (88 pounds) or more. Two on-body injectors and two prefilled cartridges are required for a full dose.
Subcutaneous injection may be self-administered, or given by caregivers, after training from a healthcare provider. The injection may be given into the abdomen, thigh, or upper arm region. Injection sites should be changed regularly, and areas where the skin is irritated, damaged, or scarred should be avoided. The two on-body injectors can be used at the same time or sequentially.
Each injection will take about 10 minutes. After that, the patient should monitor for signs or symptoms of injection-site reactions for at least one hour.
Ultomiris prefilled cartridges and on-body injectors should be stored in the refrigerator at 2-8 C (36-46 F) in their original carton protected from light. These products should never be frozen nor shaken. They can be kept at room temperature for up to three days.
Ultomiris in clinical trials
The safety and efficacy of intravenous Ultomiris in adults with PNH was assessed in two multicenter, open-label, randomized Phase 3 trials: one called ALXN1210-PNH-301 and the other ALXN1210-PNH-302. In children with PNH, the therapy’s safety and efficacy were evaluated in a Phase 3 trial called ALXN1210-PNH-304.
Another Phase 3 trial, called ALXN1210-PNH-303, evaluated the pharmacological properties of subcutaneous Ultomiris when compared with intravenous Ultomiris in adults with PNH.
ALXN1210-PNH-301
ALXN1210-PNH-301 (NCT02946463) enrolled 246 adults who had never been treated with a complement inhibitor — thus known as treatment-naïve.
Participants were randomly assigned to one of two treatment groups for a period of 26 weeks, or six months. One group received a loading dose of Ultomiris, followed by maintenance doses given every eight weeks, while the other was given five initial doses of Soliris, followed by maintenance doses given every two weeks.
At the end of the 26 weeks, patients had the option to enter the study’s extension period, during which all received Ultomiris for up to five years.
Primary study goals included assessing the number of patients remaining transfusion-free and the proportion of those achieving normalization of lactate dehydrogenase (LDH) levels in the blood. LDH is a marker of hemolysis. Secondary goals included assessing the number of patients with breakthrough hemolysis — at least one new or worsening sign of hemolysis — stabilized hemoglobin, and change in free C5 levels in the blood. Free C5 levels lower than 0.5 micrograms per milliliter (mcg/mL) indicate complete inhibition of C5 activity. Hemoglobin is the protein in red blood cells that is responsible for oxygen transport.
The results showed that Ultomiris was not inferior to Soliris for all trial goals assessed after six months of treatment. The proportion of patients achieving transfusion avoidance was similar in both groups (73.6% vs. 66.1%), as was the proportion of those attaining normalization of LDH levels (53.6% vs. 49.4%). LDH levels dropped by about 76% in both treatment groups.
More patients on Ultomiris had stabilized hemoglobin compared with those receiving Soliris (68.0% vs. 64.5%), and less patients on Ultomiris had breakthrough hemolysis (4.0% vs. 10.7%). A similar safety profile also was observed between the two therapies. Moreover, in contrast to Soliris, Ultomiris provided immediate and sustained C5 inhibition throughout the whole treatment period. Similar observations were made for patients followed up to one year.
ALXN1210-PNH-302
The trial ALXN1210-PNH-302 (NCT03056040) tested Ultomiris in adults with PNH who were clinically stable after having been treated with Soliris for at least six months. The 195 enrolled patients were randomly assigned to either continue treatment with Soliris or to switch to Ultomiris for 26 weeks. At the end of this period, patients had the option to enter the study’s extension period, during which all were given Ultomiris for up to three years.
The primary efficacy goal of the trial was assessing the percentage change in LDH. Secondary goals included assessing the proportion of patients with breakthrough hemolysis, as well as the percentage of those achieving transfusion avoidance, and stabilized hemoglobin. Changes in free C5 levels in the blood also were assessed.
Data showed that Ultomiris was not inferior to Soliris in all endpoints analyzed after six months. This included the percentage change in LDH, which dropped by 0.82% in Ultomiris-treated patients and rose by 8.4% in those given Soliris. The breakthrough hemolysis rate was 0% in the Ultomiris group and 5.1% in the Soliris group. A higher percentage of patients treated with Ultomiris achieved transfusion avoidance (87.6% vs. 82.7%) and attained stabilized hemoglobin (76.3% vs. 75.5%) compared with Soliris.
All patients receiving Ultomiris had mean free C5 levels below 0.5 mcg/mL after the first infusion and at all following visits, which was not regularly observed in those given Soliris.
Overall, study findings showed that patients with PNH may be safely and effectively switched from Soliris, given every other week, to Ultomiris administered every eight weeks. Similar observations were made for patients followed up to one year.
ALXN1210-PNH-304
The approval of Ultomiris in children with PNH was supported by data from ALXN1210-PNH-304 (NCT03406507). This 26-week study enrolled 13 children, ages 12-17. Eight were previously treated with Soliris and five had never been treated with a complement inhibitor. All patients received Ultomiris according to a weight-based dosing regimen.
The participants received a loading dose on the first day. This was followed by maintenance doses on day 15 and either once every eight weeks thereafter for those weighing at least 20 kg, or once every four weeks for those weighing less than 20 kg. The trial’s endpoints were similar to those of trials involving adults.
Interim data from the study showed that none of the patients had free C5 levels equal or higher than 0.5 mcg/mL nor experienced breakthrough hemolysis. Also, a 47.9% reduction in LDH levels was observed in complement inhibitor-naïve patients. All of the patients also experienced a clinically relevant decrease in fatigue over the course of the study. Moreover, it was found that 84.6% achieved transfusion avoidance and 69.2% had stabilized hemoglobin levels.
ALXN1210-PNH-303
The ALXN1210-PNH-303 (NCT03748823) trial was designed to assess whether Ultomiris’ pharmacological properties were identical when the medication was given by an under-the-skin injection as compared with an intravenous infusion.
The study enrolled 136 adults with PNH who were clinically stable after having received treatment with Soliris for at least three months prior to entering the trial. The patients were randomly assigned to receive weight-based doses of subcutaneous or intravenous Ultomiris for a period of 10 weeks, or about 2.5 months. After that, they entered an extension period in which all were treated with subcutaneous Ultomiris, given once weekly at a dose of 490 mg, for up to 172 weeks or just over three years.
Data showed the medication’s pharmacological properties were generally similar in both administration methods. When given subcutaneously, Ultomiris sustainably maintained free C5 levels below 0.5 mcg/mL. Moreover, no noticeable differences were found between the two forms of administration in regard to LDH percentage change, breakthrough hemolysis, transfusion avoidance, hemoglobin stabilization, and fatigue scores.
Overall, the trial findings indicated that patients with PNH may switch from intravenous treatment with Soliris or Ultomiris to subcutaneous Ultomiris without experiencing loss of treatment efficacy.
Common side effects of Ultomiris
The most common side effects observed in PNH patients related to treatment with Ultomiris are:
- upper respiratory tract infection
- headache
- injection site reactions
- diarrhea.
Infections
The Ultomiris label carries a boxed warning for serious meningococcal infections and sepsis, both of which can rapidly become life-threatening if not recognized and treated quickly.
Patients should be vaccinated against meningococcal disease at least two weeks before starting Ultomiris, unless the risk of delaying treatment is higher than that of developing a potential infection. After vaccination, patients should still be monitored for possible symptoms of meningococcal infections.
Healthcare providers should follow the most updated Advisory Committee on Immunization Practices (ACIP) recommendations for meningococcal vaccination in patients with complement pathway deficiencies.
People who have any other systemic infection should use Ultomiris with caution.
Infusion-related reactions
People treated with Ultomiris may develop infusion-related reactions, including potentially life-threatening reactions (anaphylaxis) and hypersensitivity reactions. Patients should be monitored over the course of infusion; if adverse reactions occur involving the heart and lungs, Ultomiris should be stopped and appropriate treatment initiated.
Allergies
The Ultomiris on-body injector has an acrylic adhesive that may cause allergies in certain patients. Those with a known allergy to acrylic adhesive may take preventive medications to avoid such allergies. In case of allergies, supportive measures should be taken.
Use in pregnancy and breastfeeding
Data on the use of Ultomiris in pregnant patients are scarce. Existing studies have not found adverse developmental issues. Animal studies, however, showed that a similar compound (an anti-C5 antibody) may be harmful to the developing fetus.
If left untreated, PNH poses risks to both the mother and fetus.
It is not known if Ultomiris passes into breast milk. Breastfeeding should be avoided during treatment and for eight months after the final dose.
PNH News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Direct oral anticoagulants prevent recurring blood clotting in PNH
- What I look for in a partner as someone living with PNH
- Finding the right PNH treatment isn’t a one-time decision
- Case: Empaveli effectively treats extravascular hemolysis in girl, 14
- Looking back on how my health journey affected my siblings
FAQs about Ultomiris
There are no clinical data on the use of Ultomiris in pregnant patients. However, a similar compound, an anti-C5 antibody, caused harm to the developing fetus in animal models. Pregnancy in women with untreated paroxysmal nocturnal hemoglobinuria is related to an increased risk of complications for both mother and fetus. Patients who are pregnant or are planning to become pregnant should discuss this issue with their healthcare providers.
Some paroxysmal nocturnal hemoglobinuria (PNH) patients may see results as early as two weeks after starting treatment with Ultomiris. The ALXN1210-PNH-301 trial showed that, in adults who had never received a complement inhibitor, Ultomiris could rapidly lower mean lactate dehydrogenase (LDH) levels within two weeks. LDH is a biomarker of hemolysis, or red blood cell destruction. Normalization of LDH levels could be achieved after four weeks. However, each patient is unique and may respond differently to treatment. Therefore, a discussion with their healthcare team can help PNH patients better understand how Ultomiris may help in their particular case.
The U.S. Food and Drug Administration (FDA) approved Ultomiris for the treatment of adults with paroxysmal nocturnal hemoglobinuria (PNH) in 2018. In 2021, its approval was expanded to children, ages 1 month and older. In addition to PNH, Ultomiris is approved in the U.S. for the treatment of atypical hemolytic uremic syndrome and generalized myasthenia gravis.
Related Articles
-
July 11, 2025 by Brandi Lewis
What I look for in a partner as someone living with PNH

 Fact-checked by
Fact-checked by