Voydeya (danicopan) for paroxysmal nocturnal hemoglobinuria
Last updated Aug. 22, 2024, by Marisa Wexler, MS

What is Voydeya for PNH?
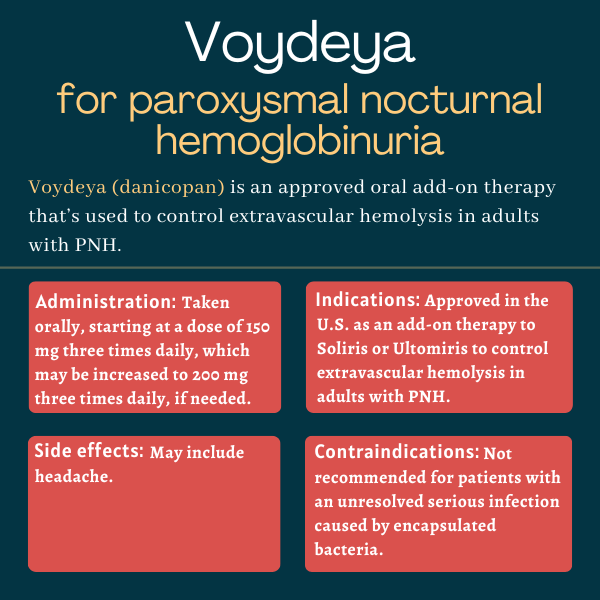
Voydeya (danicopan) is an oral medication that’s approved as an add-on treatment to Ultomiris (ravulizumab) or Soliris (eculizumab) to help treat red blood cell destruction occurring outside blood vessels in adults with paroxysmal nocturnal hemoglobinuria (PNH).
Voydeya is marketed by Alexion, AstraZeneca Rare Disease, which also sells Ultomiris and Soliris.
Therapy snapshot
| Brand name: | Voydeya |
| Chemical name: | Danicopan |
| Usage: | Add-on therapy to help treat red blood cell destruction outside blood vessels |
| Administration: | Oral tablets |
How does Voydeya work?
In PNH, a group of immune proteins in the complement system become activated and start attacking blood cells, particularly red blood cells, ultimately causing their destruction. This happens because red blood cells in PNH patients lack certain proteins on their surface that serve as identification badges signaling to the immune system that they are a healthy part of the body and should not be attacked.
All approved treatments for PNH work to block the activation of the complement cascade. Soliris and Ultomiris specifically do so by binding to a complement protein called C5, and preventing it from being cleaved or split, which is one of the steps in complement activation.
Blocking complement activation by targeting C5 is usually quite effective for stopping intravascular hemolysis (IVH), which refers to the destruction of red blood cells (hemolysis) that occurs inside blood vessels. However, these medicines aren’t as effective at stopping extravascular hemolysis (EVH), which happens when red blood cells are destroyed in tissues outside blood vessels.
About 10% to 20% of PNH patients who are taking Soliris or Ultomiris will continue to experience substantial disease symptoms due to persistent, clinically significant EVH, according to Alexion.
Voydeya is designed to target a different complement protein called Factor D, which acts upstream, or before, C5 in the cascade of complement activation. By targeting Factor D, Voydeya effectively prevents the cleavage of another complement protein called Factor B, which in turn is required for the activation of another complement protein called C3. Through this mechanism, Voydeya is expected to help prevent EVH, which is facilitated by C3, without interfering with the ability of Ultomiris and Soliris to control IVH.
Who can take Voydeya?
Voydeya was approved by the U.S. Food and Drug Administration in April 2024. The therapy is indicated to be used as an add-on treatment to Soliris or Ultomiris to help control EVH in adults with PNH. Voydeya also was approved for the same indication in Japan, the European Union, and Canada the same year.
Because Voydeya works to block the activity of part of the immune system, the medication can put patients at an increased risk of developing certain serious and life-threatening infections, particularly those caused by encapsulated bacteria.
Due to the risk of these infections, Voydeya is available in the U.S. only through Voydeya REMS, which is a restricted program to minimize the risk of serious problems from infection by ensuring proper monitoring and safety protocols are in place. REMS stands for Risk Evaluation and Mitigation Strategy and ensures that only certified healthcare providers can prescribe Voydeya while informing patients of the potential risks of treatment and making sure their vaccinations against encapsulated bacteria are up to date before treatment. The program also ensures that only certified pharmacies can dispense Voydeya.
Who should not take Voydeya?
Voydeya is contraindicated, or not recommended, for patients who have an unresolved and serious infection caused by encapsulated bacteria, including Neisseria meningitidis, Streptococcus pneumoniae, or Haemophilus influenzae type B.
It is also not recommended for patients with severe liver impairment.
The therapy’s label carries a boxed warning for serious, life-threatening infections caused by encapsulated bacteria, as these have been reported in patients treated with complement inhibitor therapies. It also notes that patients should receive vaccination against these bacteria before starting treatment with Voydeya — unless the risks of delaying Voydeya treatment outweigh the risks of developing a potentially serious infection — and that they should be monitored for early signs and symptoms of these infections while on the therapy.
Voydeya is only indicated to be used as an add-on treatment to Soliris or Ultomiris. It has not been shown to be effective when used as a monotherapy, or as a stand-alone treatment.
How is Voydeya administered?
Voydeya is available as round, white to off-white, film-coated tablets containing 50 or 100 mg of the therapy’s active ingredient. Each tablet is marked with the letters “DCN” and the dosage (50 or 100) on one side.
The tablets are to be taken orally with or without food. The recommended starting dosage is 150 mg three times per day. The dose may be increased to 200 mg three times daily if a patient required a transfusion in the previous month, or if a patient’s hemoglobin levels failed to increase as much as expected. Hemoglobin is the protein in red blood cells that’s responsible for oxygen transport.
If a scheduled dose of Voydeya is missed, patients should take the missed dose as soon as possible, unless they are within three hours of their next scheduled dose. In that case, patients should skip the missed dose and take the scheduled dose only. Patients should never take two or more doses of Voydeya at the same time.
Voydeya in clinical trials
Voydeya’s approvals were mainly supported by data from a Phase 3 clinical trial called ALPHA (NCT04469465), which evaluated the safety and efficacy of the therapy when given as an add-on treatment to Ultomiris or Soliris in a group of adults with PNH.
ALPHA trial
The study enrolled 86 adults with PNH who had substantial disease symptoms due to clinically significant EVH — defined as hemoglobin levels of 9.5 g/dL or lower, with an absolute reticulocyte count of 120 billion/L or higher, with or without transfusion support — despite being on a stable dose of Soliris or Ultomiris for at least six months. Reticulocytes are immature red blood cells.
First part
In the first part of the trial, participants were randomly assigned to receive Voydeya or a placebo for 12 weeks, or about three months, in addition to Ultomiris or Soliris. Voydeya was administered at a dose of 150 mg three times a day, which could be increased to 200 mg three times a day, depending on a patient’s clinical response.
A prespecified interim analysis was performed when 63 participants had reached the three-month mark or had discontinued treatment. The study’s main goal was to evaluate the effect of treatment on hemoglobin levels measured over the course of the first three months.
Results showed hemoglobin levels increased significantly more with Voydeya than with a placebo over the course of three months (by 2.9 vs. 0.5 g/dL). A clinically meaningful difference between Voydeya and the placebo groups was evident within two weeks after starting treatment.
Most patients (83.3%) on Voydeya did not require blood transfusions during the first three months of the trial, and more than half (59.5%) experienced an increase in hemoglobin levels of at least 2 g/dL without the need for transfusions. By comparison, about two-thirds of patients in the placebo group required transfusions during the study, and none experienced a meaningful increase in hemoglobin levels in the absence of transfusions.
Patient-reported fatigue was also assessed in the study using a 52-point scale called the Functional Assessment of Chronic Illness Therapy-Fatigue, in which higher scores indicate less fatigue. Results showed, after 12 weeks in the trial, scores improved by a mean of eight points in patients on Voydeya, and a mean of less than two points in patients on placebo.
Second part and long-term extension
After the initial placebo-controlled part of the trial, all participants were treated with Voydeya for another 12 weeks. Then, they could choose to continue receiving Voydeya as an add-on therapy given on top of Ultomiris or Soliris as part of the study’s two-year long-term extension period. Available data suggested Voydeya’s ability to increase hemoglobin levels was sustained through the trial’s second three-month treatment period and for up to about one year in total.
Ongoing trials
A Phase 3 long-term extension study (NCT05389449) is underway internationally to evaluate the long-term safety and efficacy of Voydeya when administered as an add-on therapy to Ultomiris or Soliris. The study, which will last up to three years, is enrolling PNH patients of all ages who previously took part in an Alexion-sponsored clinical trial of Voydeya. It is expected to conclude in early 2027.
Common side effects of Voydeya
The most common side effect of Voydeya observed in clinical trials is headache.
Serious infections caused by encapsulated bacteria
Voydeya carries a boxed warning noting it can increase the risk of serious and life-threatening infections caused by encapsulated bacteria such as Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type B. These infections, which have occurred in vaccinated and unvaccinated patients treated with complement inhibitors, can rapidly become life-threatening or fatal if not identified and treated early.
At least two weeks before starting treatment with Voydeya, patients should be vaccinated against encapsulated bacteria, including N. meningitidis (serogroups A, C, W, Y, and B) and S. pneumoniae. Vaccination reduces the risk of these infections, but does not completely eliminate it. Therefore, patients should be closely monitored for early signs and symptoms of such infections, and seek immediate medical attention if they experience such signs.
In cases where urgent treatment with Voydeya is needed in patients who aren’t up-to-date on their vaccines against encapsulated bacteria as recommended by guidelines, prophylactic (preventive) antibacterial therapy should be given, and the vaccines should then be administered as soon as possible afterward.
If a serious infection develops, treatment with Voydeya may be paused until the infection is resolved.
Increases in liver enzymes
Treatment with Voydeya may cause an increase in the levels of certain liver enzymes, such as alanine aminotransferase, which may be a sign of liver inflammation or damage. Liver enzyme levels should be checked before patients start treatment with Voydeya, as well as while they are on the therapy. If there are signs of clinically meaningful liver damage, treatment with Voydeya should be paused or discontinued.
Voydeya has not been studied in people with severe liver impairment, so it is not recommended for use in those patients.
Increases in cholesterol
Voydeya may cause an increase in the levels of total cholesterol and low-density lipoprotein cholesterol (commonly referred to as “bad cholesterol”). Cholesterol levels should be monitored in patients taking the therapy, and if levels rise, cholesterol-lowering medicines should be given as appropriate.
Possible hemolysis after discontinuation
If treatment with Voydeya is stopped, patients should be closely monitored for signs and symptoms of hemolysis (e.g. sudden drop in hemoglobin levels or fatigue) for at least two weeks after the last dose. Background therapy with Soliris or Ultomiris should be continued if Voydeya is stopped, or patients may be switched to another treatment. If hemolysis recurs after Voydeya has been discontinued, treatment may be restarted if appropriate.
Use in pregnancy and breastfeeding
Voydeya has not been studied in people who are pregnant or breastfeeding. Thus, it is not known whether the medication can be harmful to the developing fetus, pass into breast milk, or affect milk production or the breastfed infant.
In animal studies, the administration of Voydeya to pregnant rabbits and rats at doses much higher than the highest dose recommended for use in humans did not cause any noteworthy problems to the developing fetus. The decision of whether or not to use Voydeya during pregnancy should be made considering the potential risk of treatment, as well as the potential risks of unmanaged PNH during pregnancy.
Animal studies also suggest Voydeya is present in milk during lactation, indicating it would likely be present in breast milk, too. Since exposure to the therapy could theoretically cause problems to a breastfed infant, particularly increasing the risk of serious infection by encapsulated bacteria and causing liver enzyme levels to rise, patients are advised not to breastfeed while taking Voydeya and for at least three days after discontinuing the medication.
PNH News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- What I look for in a partner as someone living with PNH
- Finding the right PNH treatment isn’t a one-time decision
- Case: Empaveli effectively treats extravascular hemolysis in girl, 14
- Looking back on how my health journey affected my siblings
- To travel with a chronic illness, pack caution and carry courage
Related articles
-
July 11, 2025 by Brandi Lewis
What I look for in a partner as someone living with PNH