FAQs about PNH diagnosis
Paroxysmal nocturnal hemoglobinuria (PNH) can develop any age, but the disease, characterized by the lack of certain proteins on the surface of blood cells, most commonly starts and is diagnosed between the ages of 30 and 40.
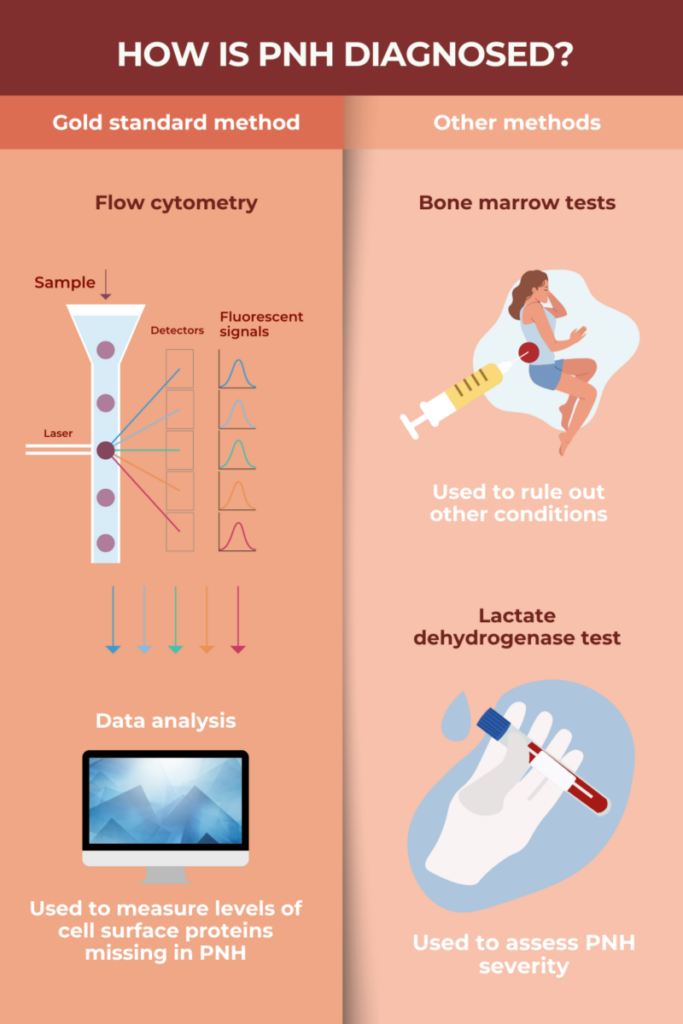
Flow cytometry is considered the gold standard method for diagnosing paroxysmal nocturnal hemoglobinuria (PNH). This type of test looks for certain proteins on the surface of blood cells, which are typically missing in people with the disorder. False-positive and false-negative test results were common a few years ago, but since then, efforts have been made to standardize the procedure and improve its sensitivity. Now, flow cytometry is considered a highly sensitive and specific test for PNH.
Paroxysmal nocturnal hemoglobinuria (PNH) has been reported in children as young as 3. However, it is more common for the disease to develop during adulthood, usually when patients are in their 30s.
Without a correct diagnosis, a person with paroxysmal nocturnal hemoglobinuria (PNH) cannot start proper treatment. As a result, the disease will continue unchecked, which can lead to severe and life-threatening complications. Without modern therapy, people with PNH typically have lived for a decade or two after disease onset. However, with modern treatments, life expectancy for someone with PNH is comparable to that of the general population.
Paroxysmal nocturnal hemoglobinuria (PNH) is usually diagnosed via flow cytometry, a test that looks for certain proteins on the surface of blood cells that are either missing or present in low levels in people with the disorder. Diagnosing aplastic anemia requires a bone marrow biopsy to assess the number of different blood cell types in the bone marrow. Flow cytometry alone cannot diagnose aplastic anemia, and a bone marrow biopsy is usually not sufficient to diagnose PNH. Given that these two conditions commonly co-occur, it’s typical for both diagnostic tests to be performed if even one of these diseases is suspected.
 Fact-checked by
Fact-checked by