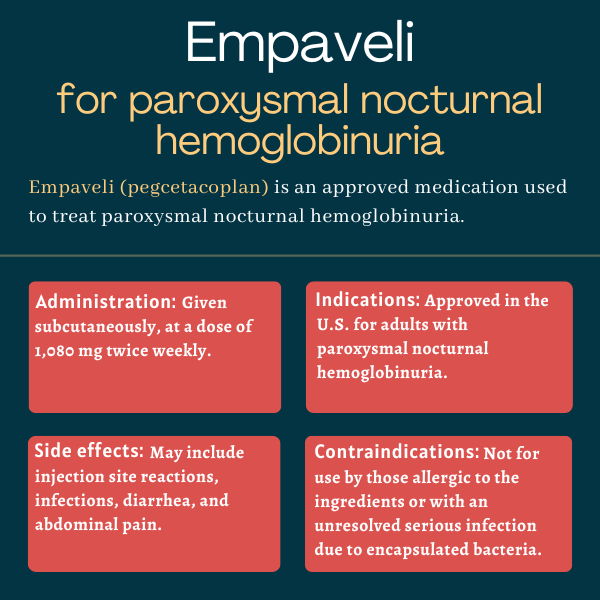
Empaveli (pegcetacoplan) for paroxysmal nocturnal hemoglobinuria
What is Empaveli for PNH?
Empaveli (pegcetacoplan) is a complement inhibitor that’s approved to treat adults with paroxysmal nocturnal hemoglobinuria (PNH). It’s given by subcutaneous (under-the-skin) injection and can be self-administered.
The therapy was developed by Apellis Pharmaceuticals and Sobi, and is marketed for PNH in Europe under the brand name Aspaveli.
Therapy snapshot
| Brand Name: | Empaveli |
| Chemical Name: | Pegcetacoplan |
| Usage: | Treatment of paroxysmal nocturnal hemoglobinuria |
| Administration: | Subcutaneous (under-the-skin) injection |
How does Empaveli work?
The complement system is a part of the immune system and helps the body fight off infections. It comprises a large number of different proteins that work together, creating a chain reaction known as the complement cascade.
A protein called C3 is a key point of the cascade, regulating its activation. This protein normally splits into two subunits: C3a and C3b. The C3b subunit is known to trigger the destruction of red blood cells outside blood vessels, usually inside the spleen or liver, in a process called extravascular hemolysis.
This subunit also activates another complement protein called C5, which is the target of two other approved PNH therapies, Soliris (eculizumab) and Ultomiris (ravulizumab). C5 also splits into two subunits: C5a and C5b, with the latter being involved in intravascular hemolysis, or the destruction of red blood cells inside blood vessels.
By preventing C3 from splitting into C3a and C3b, Empaveli helps to stop both intravascular and extravascular hemolysis, both of which are considered hallmarks of PNH.
Who can take Empaveli?
Empaveli was approved by the U.S. Food and Drug Administration in May 2021 for the treatment of adults with PNH, becoming the first and only C3-targeted therapy to earn approval for this patient population in the country.
It can be used both for patients who have never been treated before (treatment naïve) and those switching from Soliris and/or Ultomiris.
Later in the same year, the therapy was approved in Europe to treat adults with PNH who are anemic after having been treated with a C5 inhibitor for at least three months. In 2024, the therapy’s indication in Europe was extended to expand its use to treatment naïve adults with PNH.
In the U.S., Empaveli is only available through a restricted access program under a Risk Evaluation and Mitigation Strategy (REMS) due to the risk of serious infections caused by encapsulated bacteria that have been associated with treatment. The access program, called Empaveli REMS, ensures that only certified healthcare providers can prescribe Empaveli while informing patients of the potential risks of infection and making sure their vaccinations against encapsulated bacteria are up to date before treatment. The program also ensures that only certified pharmacies can dispense Empaveli.
Who should not take Empaveli?
Empaveli is contraindicated, or not recommended, for patients who:
- have known allergies to pegcetacoplan, Empaveli’s active ingredient, or any other of its components
- have an unresolved serious infection caused by encapsulated bacteria, including Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae type B.
The therapy’s label carries a boxed warning for serious, life-threatening infections caused by encapsulated bacteria, as these have been reported in patients treated with complement inhibitor therapies. It also notes that patients should receive vaccination against these bacteria before starting treatment with Empaveli — unless the risks of delaying treatment outweigh the risks of a possible serious infection. Individuals given the medication also should be carefully monitored for early signs and symptoms of infections while taking it.
How is Empaveli administered?
Empaveli is supplied in single-dose vials containing 20 mL of a colorless to slightly yellowish solution. It is given subcutaneously at a recommended dose of 1,080 mg twice weekly, using a commercially available infusion pump or the single-use, disposable Empaveli Injector.
The treatment does not require visits to an infusion center, as it can be self-administered by patients or by a caregiver after proper training. A healthcare provider should show patients or caregivers how to prepare and administer the treatment before they attempt to do so.
When using an infusion pump, Empaveli is administered with a small, thin needle that can be placed in either one or two sites on the abdomen, thighs, hips, or upper arms. The Empaveli Injector is exclusively used to administer the therapy into the abdomen. Regardless of which administration method is used — the infusion pump or the Empaveli Injector — patients should rotate administration sites, and avoid injecting the medication in regions where the skin is tender, bruised, red, or hard. Sites with tattoos, scars, or stretch marks also should be avoided.
Each infusion done with a commercially available infusion pump usually takes around 30 minutes if patients use two injection sites; it generally takes about 60 minutes, or one hour, if they use only one site. Each injection given through the Empaveli Injector takes normally 30 to 60 minutes to complete.
Before use‚ Empaveli should reach room temperature for approximately 30 minutes. Until then, medication vials should be kept inside their carton and protected from light.
It is recommended that patients switching from C5 inhibitors do not discontinue these treatments abruptly when starting Empaveli so as to reduce the risk of hemolysis, or red blood cell destruction. Those switching from Soliris are advised to discontinue this therapy only four weeks (one month) after starting treatment with Empaveli. Patients switching from Ultomiris are recommended to start Empaveli no more than four weeks after their last dose of Ultomiris.
Lactate dehydrogenase (LDH) is a marker of hemolysis. In patients in whom LDH levels are two times higher than the upper limit of normal, Empaveli’s dosing regimen should be adjusted to 1,080 mg given every three days. LDH levels should be monitored twice weekly for at least four weeks in case there is an increase in treatment dosage.
If a scheduled dose of Empaveli is missed, patients should take the missed dose as soon as possible and resume their regular dosing schedule thereafter.
Empaveli in clinical trials
The safety and efficacy of Empaveli in adults with PNH were evaluated in two Phase 3 clinical trials. One, called PEGASUS, enrolled patients previously treated with Soliris, while the other, known as PRINCE, involved adults who had not been previously treated with a complement inhibitor.
PEGASUS trial
PEGASUS (NCT03500549), completed in 2020, assessed the efficacy and safety of Empaveli in 80 adults with PNH who were being treated with Soliris. To be eligible to participate in the study, patients had to have been on a stable dose of Soliris for at least three months before entering the trial. Additionally, their hemoglobin levels had to be lower than 10.5 g/dL; hemoglobin is the protein in red blood cells that’s responsible for oxygen transport.
Patients started by receiving both treatments for four weeks. After that, they were randomly assigned to receive either Empaveli or Soliris for 16 weeks. Finally, patients were allowed to either continue or switch to Empaveli for an extension period of 32 or 28 weeks, respectively.
The trial’s primary goal was assessing changes in hemoglobin levels from the beginning of the study (baseline) until week 16. Further clinical and blood markers of hemolysis also were evaluated, as was treatment safety.
Results showed Empaveli outperformed Soliris in its ability to maintain or increase hemoglobin levels. In Empaveli-treated patients, hemoglobin levels rose by a mean of 2.37 g/dL over the course of 16 weeks, while in Soliris-treated patients they fell by a mean of 1.47 g/dL — a difference of 3.84 g/dL favoring Empaveli.
The majority of patients (85%) treated with Empaveli no longer needed blood transfusions — a procedure normally required to treat anemia due to hemolysis. In patients receiving Soliris, however, only 15% of patients no longer required blood transfusions. Empaveli also was found to ease fatigue.
Findings from the extension part of the trial also showed that hemoglobin levels remained sustainably higher in patients who remained on Empaveli over 48 weeks, or nearly one year.
PRINCE trial
PRINCE (NCT04085601) assessed the efficacy and safety of Empaveli in comparison to standard therapies in 53 adults with PNH who had not been previously treated with a complement inhibitor. To be eligible for this trial, patients must not have been treated with any complement inhibitor in the three months leading up to study entry. Additionally, their hemoglobin levels had to be below the lower limit of normal and LDH levels had to be above the upper limit of normal.
Participants were randomly divided into two groups and assessed for 26 weeks, or around six months. In one of the groups, patients were given Empaveli, while in the other group they continued receiving standard PNH supportive treatment (control group), which might include blood transfusions, corticosteroids, iron, folate, and vitamin B12 supplements.
The study’s main goals included assessing the proportion of patients achieving hemoglobin stabilization after 26 weeks of treatment, as well as evaluating changes in LDH levels over the same period of time.
Results showed most people in the Empaveli group achieved hemoglobin stabilization throughout the study period, while none of the patients in the control group did (85.7% vs. 0%). A higher reduction in mean LDH levels was observed within two weeks in the Empaveli group compared with the control group, which was sustained over the entire 26-week study period.
Ongoing trials
A Phase 3 open-label extension study (NCT03531255) is assessing the long-term safety and efficacy of Empaveli in PNH patients who previously participated in, and completed, other Empaveli studies, including the PEGASUS and PRINCE trials. Patients enrolling in the extension study are receiving Empaveli at a dose of 1,080 mg twice weekly, every three days, or three times a week.
Available 48-week data from the extension study showed that Empaveli maintained hemoglobin levels close to 12 g/dL, eased fatigue, and reduced patients’ dependence on transfusions. The extension study is still ongoing and expected to conclude in 2025.
A Phase 2 trial (NCT04901936) also is evaluating the safety and effectiveness of Empaveli in children and adolescents, ages 12-17, with PNH.
Participants are screened for four weeks and then treated for 16 weeks — for a total time period of about five months. Those switching from a C5 inhibitor will have an additional run-in period of four weeks between screening and treatment. At the end of the treatment period, participants will either enter a long-term extension period or a follow-up period for two months. All participants will be given Empaveli by subcutaneous infusion twice weekly at home.
Primary outcome measures include assessing changes in blood levels of Empaveli, hemoglobin, and LDH over the 16-week period. Secondary goals include evaluating changes in several parameters over the extension part of the study. These include C3 levels on red blood cells, incidence of blood-clotting events and hemolysis, hemoglobin levels, and quality of life.
The trial is expected to conclude in October 2024.
Common side effects of Empaveli
The most common side effects related to Empaveli are:
- injection-site reactions
- infections
- diarrhea
- abdominal pain
- respiratory tract infection
- pain in the hands and feet
- low levels of potassium in the blood (hypokalemia)
- fatigue
- viral infection
- cough
- joint pain (arthralgia)
- dizziness
- headache
- rash.
Serious infections caused by encapsulated bacteria
The Empaveli label carries a boxed warning for serious infections and for life-threatening infections caused by encapsulated bacteria, such as Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type B. Empaveli can increase the risk of these infections, which can rapidly become life-threatening if not recognized and treated quickly.
To reduce this risk, all patients should be vaccinated against these bacteria, including N. meningitidis (serogroups A, C, W, Y, and B) and S. pneumoniae, at least two weeks before starting treatment with Empaveli. That’s according to the most updated Advisory Committee on Immunization Practices (ACIP) recommendations for patients with complement deficiencies. Those who are already vaccinated are recommended to receive a booster dose if needed, depending on treatment duration.
If Empaveli has to be started immediately in patients who aren’t up to date on their vaccines against encapsulated bacteria as recommended by guidelines, preventive antibacterial treatment should be given. Vaccines should then be administered as soon as possible.
Patients should be closely monitored for early signs of infection and evaluated immediately if an infection is suspected. Therapy discontinuation should be considered if patients are being treated for serious infections.
Infusion-related reactions
People treated with Empaveli may develop infusion-related reactions, including hypersensitivity and potentially life-threatening reactions, known as anaphylaxis. If a severe hypersensitivity reaction occurs, Empaveli should be stopped and appropriate treatment initiated.
Possible hemolysis after discontinuation
If Empaveli is stopped, patients should be closely monitored for signs and symptoms of hemolysis for at least eight weeks. Among these signs and symptoms may be a sudden drop in hemoglobin levels coupled with elevated LDH levels, fatigue, and other symptoms. If hemolysis recurs after Empaveli has been discontinued, treatment may be restarted if appropriate.
Use in pregnancy and breastfeeding
Studies on the use of Empaveli in pregnant women are still lacking. Studies in primates indicated that the treatment may cause harm to a developing fetus. Patients who are pregnant or are planning to become pregnant should discuss the subject with their healthcare team.
It is not known whether Empaveli passes into human breast milk or if it affects milk production. However, traces of Empaveli were found in the breast milk of monkeys. As many compounds pass into human breast milk and potentially cause serious side effects in a nursing child, Empaveli’s label recommends breastfeeding should be stopped during treatment and for 40 days after the last dose.
PNH News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- New questionnaire assessing fatigue ‘reliable and valid’ for adults with PNH
- Progress in research and treatments is a reason for holding on to hope
- New gene study highlights clot risk factor in people living with PNH
- Becoming a patient advocate gave me purpose in the fight against PNH
- Study finds Ultomiris safe as PNH treatment during pregnancy
FAQs about Empaveli
The interaction between alcohol and Empaveli has not been established. However, since alcohol can interfere with some medications, patients are recommended to talk with their healthcare team about the potential effects of alcohol while on Empaveli.
There is a lack of data on the use of Empaveli in pregnant women. Studies in monkeys indicated the treatment may cause harm to the developing fetus. Patients who are pregnant or are planning to become pregnant should discuss this issue with their healthcare providers.
Neither hair loss nor weight gain have been reported in clinical trials as adverse effects associated with Empaveli. Patients are recommended to talk with their healthcare team if they develop any unusual symptoms while on the medication.
Some persons with paroxysmal nocturnal hemoglobinuria (PNH) may see results as early as two weeks after starting treatment with Empaveli. The PRINCE trial showed that, in adults who had never received a complement inhibitor, Empaveli could rapidly lower mean lactate dehydrogenase (LDH) levels within two weeks. LDH is a biomarker of hemolysis, or red blood cell destruction. However, each patient is unique and may respond differently to treatment. Therefore, a discussion with their healthcare team can help PNH patients better understand how Empaveli may help in their particular case.
Empaveli was approved by the U.S. Food and Drug Administration (FDA) in 2021 for use in adults with paroxysmal nocturnal hemoglobinuria (PNH), including those who had never been treated before and those switching from Soliris (eculizumab) and/or Ultomiris (ravulizumab).
 Fact-checked by
Fact-checked by