FDA reviewing application requesting approval of crovalimab
Treatment would be given via subcutaneous injection every 4 weeks

The U.S. Food and Drug Administration (FDA) has agreed to review an application seeking the approval of the monthly subcutaneous (under-the-skin) injection therapy crovalimab as a treatment for paroxysmal nocturnal hemoglobinuria (PNH), according to its developer, Genentech.
“This filing acceptance reinforces the value of crovalimab,” Levi Garraway, MD, PhD, chief medical officer and head of global product development at Genentech, a Roche member, said in a company press release.
Genentech did not specify in its announcement when a final decision from the FDA is expected. Typically, the U.S. agency announces decisions on therapy approvals about 10 months after an application is accepted.
“If approved, crovalimab will be the first monthly subcutaneous treatment for PNH, with the option to self-administer outside of a supervised healthcare setting. This filing acceptance is another step towards bringing a new treatment option, which has the potential to address the high burden of a disease that requires lifelong treatment, to PNH patients and their caregivers,” Juliana Lagrasta Biondo, MD, executive medical director of oncology/hematology at Genentech, said in an emailed statement to PNH News.
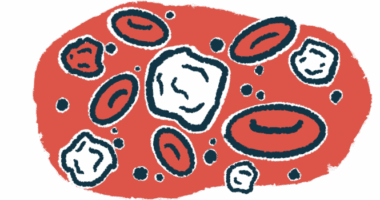
In PNH, a part of the immune system called the complement cascade becomes abnormally activated, leading to hemolysis, or blood cell destruction, ultimately driving disease symptoms. There are several available treatments for PNH; all of them work to block the activation of the complement cascade.
Like other PNH treatments, crovalimab also works by stopping complement activation. The therapy specifically targets a complement protein called C5. The approved PNH treatments Soliris (eculizumab) and Ultomiris (ravulizumab), both marketed by AstraZeneca, also work by targeting C5.
Soliris is given by infusion into the bloodstream every other week, while Ultomiris can be administered by infusion every eight weeks, or by a weekly subcutaneous injection (in adults only). Crovalimab is designed to be given by subcutaneous injection every four weeks, which can be done by patients or caregivers at home.
“Crovalimab could provide an option to self-administer as infrequently as every four weeks, thereby reducing clinic visits for people with this lifelong condition,” Garraway said, adding that the therapy “was engineered to be recycled in the bloodstream with the goal of offering a sustained response while reducing treatment burden.”
Application based on data from clinical trials
Genentech’s application seeking the approval of crovalimab is based primarily on data from the Phase 3 COMMODORE 2 trial (NCT04434092), which tested crovalimab against Soliris in people with PNH who had not previously been on a complement-blocking therapy.
Results showed that both treatments were comparable at stopping hemolysis. Safety data also were comparable; side effects were reported in about four out of five patients given either treatment.
Genentech’s application also included data from another Phase 3 clinical trial, called COMMODORE 1 (NCT04432584), which is testing crovalimab in people who had previously been treated with Soliris or Ultomiris. Available data from the study have generally indicated that switching from either approved therapy to crovalimab did not result in a notable increase in disease activity.
Data from other clinical trials, including the Phase 1/2 COMPOSER study (NCT03157635) and the Phase 3 COMMODORE 3 trial (NCT04654468), have generally suggested that crovalimab can effectively reduce hemolysis, limit the need for blood transfusions, and lessen fatigue in people with PNH.
Crovalimab also is being considered for approval as a PNH treatment in Japan, China, and Europe.