Abnormal NK cells may disrupt immune activity in PNH: Study
Patients show abnormalities in infection-fighting immune cells
Written by |
People with paroxysmal nocturnal hemoglobinuria (PNH) have abnormalities in infection-fighting immune cells called natural killer (NK) cells, a study showed, shedding light on how this blood cell disorder may dysregulate the immune system.
The study, “Role of NK cells in immune escape in patients with classical paroxysmal nocturnal haemoglobinuria,” was published in Clinical and Translational Medicine.
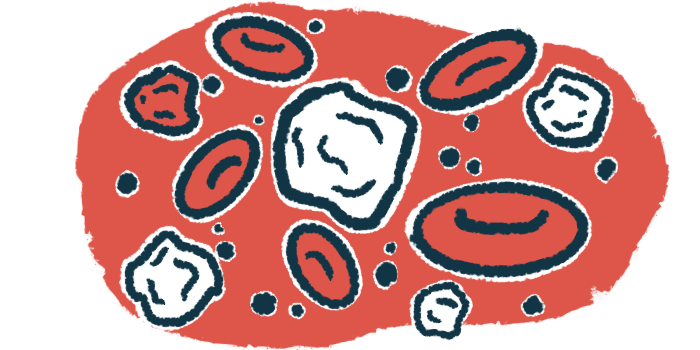
PNH is caused by defects in hematopoietic stem cells (HSCs), which reside in the bone marrow and are responsible for producing new blood cells. These defective HSCs result in blood cells that lack certain surface molecules. The main consequence is that red blood cells (the cells that carry oxygen) are abnormally destroyed, which drives PNH symptoms such as anemia.
In addition to red blood cells, HSCs make infection-fighting white blood cells, including NK cells. As their name implies, these cells act as the body’s hitmen, killing off threats such as infectious bacteria, participating in cancer immunosurveillance, and playing a role in autoimmune diseases. Little is known about how NK cells are affected by PNH.
Analyzing NK cells
To learn more, scientists in China conducted detailed analyses of NK cells from 26 people with PNH. NK cells from 27 people without PNH were also evaluated for comparison. Overall, the researchers found that NK levels were lower in PNH patients.
Most people with PNH have healthy HSCs alongside the defective ones. As a result, PNH patients have some NK cells that express all normal surface markers, and others that lack a specific marker, CD59.
The researchers found that people with PNH have lower-than-normal numbers of mature NK cells, not only in NK cells lacking CD59 but also in CD59-positive NK cells that express all the normal markers. Both types of NK cells also showed dysregulation in the activity of several inflammatory genes that are key for fighting infections, but in different directions: NK cells lacking CD59 were less inflammatory than normal, while CD59-positive NK cells elicited an increased inflammatory response by participating in mechanisms of immune escape.
In other words, these CD59-positive cells become hyperactivated, disrupting the body’s ability to control other immune cells, specifically T lymphocytes. This disruption creates a protective environment that allows the abnormal PNH clones to thrive and expand.
“In patients with classical PNH, both the quantity and function of NK cells are reduced, with significant differences in the distribution of [CD59-positive and -negative] NK cell subset,” the researchers wrote.
The results provide “novel insights into NK cell dysfunction in PNH and [highlight its] potential role in immune escape,” they said.